We respect your privacy. Unsubscribe at any time
Menopause, Muscle & Midlife Metabolism
Understanding Body Composition and Abdominal Fat Redistribution
Many women notice a shift during perimenopause or menopause that feels frustrating and confusing.
You may not be eating more.
You may still be exercising.
Yet your shape changes.
Your waistline thickens.
Your midsection feels softer.
Clothes fit differently.
This is not just about weight.
It is about body composition.
Recent research examining the menopausal transition highlights measurable changes in muscle mass and abdominal fat redistribution. Understanding these changes allows us to respond strategically rather than react emotionally.
What Is Body Composition?
Body composition refers to the proportion of:
- Lean mass, including skeletal muscle
- Fat mass
- Body water
- Bone mass
Two women can weigh the same but have very different metabolic profiles depending on muscle and fat distribution.
Menopause can influence this balance.
What Changes During the Menopausal Transition?
Across reproductive stages, postmenopausal women have been shown to demonstrate:
- Reduced lean body mass
- Reduced skeletal muscle mass
- Increased visceral fat area
- Increased waist-to-hip ratio
- Greater central fat accumulation
Importantly, total weight does not always increase dramatically. What often changes is distribution and muscle preservation.
Many women report minimal change on the scale alongside noticeable changes in waistline and body shape.
Individual variation is significant. Age, genetics, activity levels, sleep, nutrition, and metabolic history all contribute.
Why Fat Redistributes Toward the Abdomen
Oestrogen influences:
- Fat storage patterns
- Insulin sensitivity
- Energy metabolism
- Muscle protein turnover
During perimenopause and menopause:
- Fat storage may shift from hips and thighs toward the abdomen
- Visceral fat may increase
- Muscle protein synthesis may decline
- Resting metabolic rate may reduce
Visceral fat is metabolically active and is associated with increased cardiometabolic risk.
This does not mean disease is inevitable.
It does mean midlife is an important window for prevention.
The Overlooked Factor: Muscle Loss
From midlife onward, women commonly experience gradual loss of skeletal muscle, which may become more noticeable after menopause.
Reduced muscle mass is associated with:
- Lower metabolic efficiency
- Reduced insulin sensitivity
- Increased fat storage
- Reduced strength and balance
- Increased long term fracture risk
Muscle is not simply aesthetic.
It plays an important role in metabolic health and long term resilience.

Journal Club
The Impact of the Menopausal Transition on Body Composition and Abdominal Fat Redistribution (2026)
Szeliga A, Chedraui P, Meczekalski B
Study design
Cross-sectional analysis of women across reproductive stages using bioelectrical impedance to assess body composition.
What was examined
Lean body mass
Skeletal muscle mass
Visceral fat area
Waist-to-hip ratio
Total body water
Key findings
Compared to premenopausal women, postmenopausal women demonstrated:
- Lower lean body mass
- Lower skeletal muscle mass
- Higher visceral fat area
- Greater central fat accumulation
Differences in total body weight were not always substantial.
The most significant change observed was redistribution and muscle reduction rather than simple weight gain.
Why this matters clinically
Central fat accumulation and reduced muscle mass are associated with increased cardiometabolic risk and long-term functional decline.
These findings support a shift away from focusing solely on the scale and toward preserving muscle while monitoring central adiposity during midlife.
How this informs practice
Evidence-informed midlife care may include:
- Prioritising muscle preservation
- Monitoring central adiposity trends
- Avoiding over-reliance on weight alone
- Supporting cardiometabolic risk screening where clinically indicated
This is not about alarm. It is about proactive strategy.
Limitations of the Study
Cross-sectional design
Age as a confounding variable
Bioimpedance precision limitations
Menopause is likely one contributor within a broader ageing and lifestyle context.
A Practical 3 Step Framework
1. Think Strength First
Resistance training 2-3 times per week is associated with:
- Muscle preservation
- Improved insulin sensitivity
- Bone density support
- Metabolic efficiency
This can be gym-based or home-based. Consistency matters more than complexity.
2. Optimise Protein Intake
Baseline Australian recommendations are approximately 0.75 g/kg/day.
For midlife muscle preservation, intake often sits closer to:
1.0–1.2 g/kg/day
and in some contexts 1.2–1.5 g/kg/day, depending on training and health status.
Distribute protein across meals rather than concentrating intake at dinner.
3. Monitor Central Adiposity
Waist circumference is used in Australian cardiovascular risk assessment.
For women:
- ≥ 80 cm is associated with increased chronic disease risk
≥ 88 cm is associated with substantially higher risk
Tracking change over time is often more useful than a single measurement.
If waist circumference is rising or above 80 cm, a review of lifestyle and cardiometabolic markers may be appropriate.
Individualised assessment remains central to safe and effective care.
A Final Thought
Menopause is not a failure of willpower.
It is a biological transition.
Midlife is an opportunity to invest in strength, metabolic health and long-term resilience.
You are not behind.
You are adapting.
You’re not alone on this journey — and understanding how different treatments work can support more informed, confident decisions.
If you’d like support or a personalised review, you’re welcome to reach me at:
📧 hello@menopauseandme.com.au
🌐 www.menopauseandme.com.au
Warmly,
Jenna
Nurse Practitioner & Menopause Educator
Sources
Szeliga A, Chedraui P, Meczekalski B. The Impact of the Menopausal Transition on Body Composition and Abdominal Fat Redistribution. 2026. | Australasian Menopause Society. Weight management and healthy ageing information sheets. | Australian Heart Foundation, 2026. What waist measurements mean for your heart | International Menopause Society. White Paper on Lifestyle Medicine in Menopausal Health, 2025.| ESPEN and PROT-AGE Study Group. Protein intake recommendations for older adults. | North American Menopause Society. Position statements on menopause and metabolic health.
Journal Club feature:
Szeliga, A., Chedraui, P., & Meczekalski, B. (2026). The impact of the menopausal transition on body composition and abdominal fat redistribution. Journal of Clinical Medicine, 15(2), 740. https://doi.org/10.3390/jcm15020740
Important Disclaimer: The information in this blog/newsletter is general in nature and intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your Nurse Practitioner, doctor, or another qualified health practitioner with any questions you may have regarding a medical condition or before commencing any new treatment, exercise program, changing your diet, or taking supplements – particularly if you have existing health conditions, are on medication, or have had fractures or falls in the past. Individual needs and responses vary.
The Combined Oral Contraceptive Pill and Perimenopause
What’s Really Happening With Your Hormones?
Hello and welcome to Menopause & Me.
I’m Jenna, Nurse Practitioner and menopause educator.
Many women in perimenopause still require reliable contraception or support with cycle control. For this reason, the combined oral contraceptive pill (COCP) is commonly prescribed during midlife.
As women move through perimenopause, however, hormonal needs can change — and the combined pill works very differently from menopause hormone therapy (MHT). Understanding this difference can help explain why some women notice unexpected or new symptoms during this stage of life.
This article explores how the combined pill works, how it differs from menopause hormone therapy, and why a review can be helpful as needs evolve.

How the combined pill works
The combined oral contraceptive pill contains:
- A synthetic progestogen (progestin)
- A synthetic oestrogen (most commonly ethinylestradiol)
Its primary actions are to:
- Suppress ovulation
- Reduce the ovaries’ natural production of oestradiol, progesterone, and testosterone
This creates a steady, non-cyclical hormonal environment. Although a monthly withdrawal bleed may occur, this does not reflect a natural ovulatory cycle.

Why the combined pill is not menopause hormone therapy
Menopause hormone therapy aims to support symptoms associated with hormonal decline by replacing oestradiol (and progesterone when required) using body-identical hormones at physiological doses.
In contrast, most combined oral contraceptive pills:
- Contain synthetic hormones rather than body-identical forms
- Suppress ovarian hormone production rather than replacing it
- Are designed for contraception and cycle control, not menopausal symptom management
For these reasons, the combined pill is not considered a form of menopause hormone therapy.
Effects on oestrogen levels
Despite containing oestrogen, many combined pills result in relatively low circulating oestradiol levels compared with typical physiological midlife requirements.
For some women, this may be associated with symptoms such as:
- Hot flushes or night sweats
- Vaginal dryness or discomfort
- Changes in sleep quality
Individual responses vary, and not all women experience these effects. Symptoms are influenced by many factors beyond oestrogen alone.
Effects on progesterone and mood
Because ovulation is suppressed while taking the combined pill, the body produces little natural progesterone.
Progesterone plays a role in:
- Sleep regulation
- Mood stability
- Nervous system calming
Lower endogenous progesterone levels may be associated with sleep disturbance, anxiety, or low mood in some women, though these symptoms are always multifactorial and individual.
Effects on testosterone and sexual wellbeing
The combined pill may:
- Reduce ovarian testosterone production
- Increase sex hormone-binding globulin (SHBG), which lowers free testosterone levels
For some women, this can influence sexual desire, energy, motivation, or overall wellbeing. These effects are variable and not universal.
When the combined pill may still be appropriate
The combined pill can remain an appropriate option for some women who need:
- Reliable contraception
- Management of heavy or irregular bleeding
- Hormonal support in premature ovarian insufficiency or early menopause
Newer formulations containing estradiol or estetrol may be better tolerated for some women. These options remain contraceptive treatments rather than menopause hormone therapy.
As with all hormonal options, the benefits and risks should be reviewed in the context of age, medical history, and personal priorities. A personalised review is essential.
Journal Club: Placing the evidence in context
As part of our commitment to evidence-based menopause care, we also share selected research through Journal Club at Menopause & Me.
For this topic, we’ve highlighted a recent 2025 peer-reviewed review examining the use of hormonal contraception, including the combined oral contraceptive pill, in perimenopausal women. The paper is important because it helps explain why advice about the combined pill can differ between clinicians and why guidance has changed over time.
The review shows that evidence in this area is still evolving, particularly for women in later reproductive years, and that many recommendations are based on expert consensus rather than definitive trial data. It reinforces that the combined pill may still be appropriate for some women, but it is not menopause hormone therapy and does not suit everyone.
Importantly, this research supports current practice moving away from blanket rules and towards regular review, individual risk assessment, and shared decision-making as women’s needs change through perimenopause.
You don’t need to read research papers yourself — Journal Club is simply a way of translating evidence into clear, relevant context to support informed conversations about care.
A simple 3-step check-in
If you’re using the combined pill during perimenopause, it may be helpful to:
- Notice any changes in symptoms (bleeding, mood, sleep, flushes, libido)
- Book a consultation with a menopause-trained healthcare provider
- Ask:
“Is the combined pill still the best option for my contraceptive and symptom needs at this stage of life?”
You’re not alone on this journey — and understanding how different treatments work can support more informed, confident decisions.
If you’d like support or a personalised review, you’re welcome to reach me at:
📧 hello@menopauseandme.com.au
🌐 www.menopauseandme.com.au
Warmly,
Jenna
Nurse Practitioner & Menopause Educator
Sources
Australasian Menopause Society – Contraception and Perimenopause | Faculty of Sexual & Reproductive Healthcare – Combined Hormonal Contraception Guidelines | British Menopause Society – Midlife Hormone Guidance | Prior JC et al. – Progesterone physiology and perimenopause | Panay N et al. – Hormonal contraception in midlife women
Journal Club feature:
Whitburn, S., McNamee, K., Boerma, C., & Bateson, D. (2025). Hormonal contraception in perimenopausal women. Best Practice & Research Clinical Obstetrics & Gynaecology, 103, 102655. https://doi.org/10.1016/j.bpobgyn.2025.102655
Important Disclaimer: The information in this blog/newsletter is general in nature and intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your Nurse Practitioner, doctor, or another qualified health practitioner with any questions you may have regarding a medical condition or before commencing any new treatment, exercise program, changing your diet, or taking supplements – particularly if you have existing health conditions, are on medication, or have had fractures or falls in the past. Individual needs and responses vary.
Why Menopause Care Is Evolving and Why Evidence Matters
Menopause care is not broken, but it is changing.
For a long time, menopause was treated as something women simply had to endure. Symptoms were often minimised, normalised, or dismissed as “just part of getting older”.
Many women were told there was little that could be done, or that treatment options were unsafe or unnecessary. That story is changing. Not because of trends or social media, but because the evidence base around menopause has grown and matured.
Modern menopause care looks different to what many women were told years ago, and that can feel confusing. This article explains why menopause care is evolving, what evidence-based care really means, and how to make sense of changing information.
What does evidence-based menopause care actually mean?

Evidence-based care means that decisions are guided by three key elements:
• The best available medical research
• Clinical guidelines that are regularly reviewed and updated
• A woman’s individual symptoms, health history, risk factors, and treatment goals
Importantly, evidence-based care does not mean there is one correct approach for everyone.
It does not mean:
• Everyone should use hormone therapy
• Blood tests tell the full story
• Symptoms should be ignored if results are “normal”
Instead, it supports individualised care and shared decision-making.
Why menopause evidence has historically been limited
Menopause research has not always kept pace with other areas of medicine.
Contributing factors include:
• Women being under-represented in older clinical trials
• Early studies using hormone formulations that are no longer commonly prescribed
• Long-lasting fear following early 2000s data that was later re-interpreted
• Limited research focused on quality-of-life outcomes rather than disease alone
As research methods improve and newer treatments are studied, our understanding evolves. This does not mean previous clinicians were negligent. It means medicine responds as better data becomes available.
What has changed in modern menopause care?
A stronger focus on symptoms and lived experience
In perimenopause, hormone levels can fluctuate significantly. For many women, a single hormone blood test may not reflect what is happening day to day, so symptoms, patterns, and impact on daily life are often more helpful in guiding care.
A clearer understanding of hormone therapy
Modern menopausal hormone therapy is different to what many women remember hearing about in the past. Current practice often involves individualised options such as:
• Lower doses
• Where clinically appropriate, transdermal oestrogen
• Micronised progesterone
• Risk assessment based on the individual rather than blanket rules
For some women, hormone therapy is appropriate and beneficial. For others, non-hormonal strategies are a better fit.
Recognition of non-hormonal support
Menopause care may also include lifestyle strategies, sleep support, mental health care, vaginal therapies, non-hormonal medications, education, and reassurance. Hormones are one option, not the only option.
Why guidelines change and why that matters
Clinical guidelines are not static. They are updated as new evidence emerges and older assumptions are reviewed.
Menopause guidance is informed by organisations such as the Australasian Menopause Society, the International Menopause Society, and international health bodies including NICE.
When advice changes, it is not because someone was wrong. It is because we now understand more than we did before.
Why menopause information can feel overwhelming
Menopause affects sleep, mood, work, relationships, confidence, and physical health. When women feel dismissed or unheard, they understandably seek answers elsewhere.
Online information can be helpful, but it can also:
• Oversimplify complex research
• Present personal experiences as universal truths
• Amplify fear or certainty where nuance is needed
Evidence-based care helps filter information through context, balance, and clinical experience.
Introducing Journal Club at Menopause & Me
As menopause research continues to grow, we believe women deserve help understanding it, not just hearing about it.
That is why we have introduced Journal Club at Menopause & Me.

Journal Club posts will be shared fortnightly on our Facebook and Instagram pages, aligned with each newsletter topic, to allow time for thoughtful discussion and reflection.
Journal Club is a way of translating menopause research into clear, patient-friendly explanations. It explores:
• What a study actually examined
• What it can and cannot tell us
• How it fits with current clinical guidelines
• What it may or may not mean for real-world care
Journal Club is not about hype, trends, or absolutes. It is about clarity, balance, and honesty, including acknowledging where evidence is still evolving.
You do not need to read research papers yourself. If you want help interpreting new information, we can translate it into plain language and place it in context.
Staying connected between newsletters
To support deeper understanding and avoid information overload, our newsletters and blog articles will now be shared on a fortnightly basis.
This allows time between editions to reflect on key topics, explore evidence through our Journal Club post, and continue conversations across our social media platforms.
Our focus remains on providing clear, evidence-based information at a pace that supports real life, not rush.
What this means for you
Modern menopause care is no longer about pushing through or accepting poor quality of life as inevitable.
You deserve:
• To feel heard
• To understand your options
• To be involved in decisions about your care
• To review and adjust approaches as your needs evolve
Evidence-based care supports thoughtful, individualised conversations rather than rushed answers.
A final thought
Menopause care is evolving because women’s health is finally being examined with greater depth, nuance, and respect.
Good care is not about chasing trends or fearing change.
It is about combining evidence, clinical experience, and individual needs, and adapting as knowledge grows.
That is how menopause care moves forward safely and confidently.
If you would like to seek further information about these symptoms or learn more about assessment options, you can contact Menopause & Me:
🌐 menopauseandme.com.au/booking
You’re not alone on this journey: knowledge is power!
Warm Regards,
Jenna Bell
Nurse Practitioner & Menopause Educator
Sources
Australasian Menopause Society | International Menopause Society | NICE Menopause Guidelines
Important Disclaimer: The information in this blog/newsletter is general in nature and intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your Nurse Practitioner, doctor, or another qualified health practitioner with any questions you may have regarding a medical condition or before commencing any new treatment, exercise program, changing your diet, or taking supplements – particularly if you have existing health conditions, are on medication, or have had fractures or falls in the past. Individual needs and responses vary.
Sleep, Mood & Brain Fog in Perimenopause and Menopause: Understanding Evidence-Based Management Pathways [Menopause Symptoms & Systems Series (Part 3 of 3)]
In Part 1, we explored why sleep and fatigue commonly change during perimenopause and menopause, and why these symptoms are often multifactorial.
In Part 2, we looked at why sleep disturbance, anxiety, low mood, and cognitive symptoms such as “brain fog” so often occur together — and why they are best understood as interconnected systems.
In Part 3, we bring this together by outlining how clinicians think about evidence-based management pathways for these symptoms, and why an individualised, stepwise approach is supported by current clinical guidance.
Why there is no single “right” treatment

Because sleep disturbance, mood changes, anxiety, and cognitive symptoms are influenced by multiple overlapping factors, there is no one-size-fits-all solution.
Management is most effective when it:
- Identifies the dominant contributors for that individual
- Prioritises symptoms that are most disruptive to quality of life
- Considers preferences, health history, and contraindications
- Uses evidence-based options in a thoughtful, staged way
This is why menopause care often looks different from person to person.
A sleep-first lens
Sleep is often a key driver of other symptoms.
Fragmented or insufficient sleep can worsen:
- Anxiety and emotional reactivity
- Low mood
- Concentration and memory efficiency
- Stress tolerance
For this reason, clinical assessment frequently starts with understanding sleep patterns and contributors, even when mood or cognitive symptoms are the primary concern.
Non-pharmacological approaches
Insomnia-focused therapies
For women experiencing persistent insomnia, cognitive behavioural therapy for insomnia (CBT-I) is recognised as a first-line, evidence-based approach.
CBT-I focuses on:
- Sleep behaviours and routines
- Sleep drive and circadian timing
- Thought patterns that perpetuate insomnia
International guidance recognises CBT-I — including menopause-specific CBT approaches — as appropriate for menopause-related sleep disturbance.
Lifestyle and behavioural strategies
Supportive strategies may include:
- Establishing consistent sleep–wake times
- Reducing factors that fragment sleep (such as alcohol sensitivity)
- Managing cognitive and emotional load
- Supporting stress regulation
These approaches are often used alongside other management options.
Hormonal therapy considerations
Hormonal changes during the menopause transition can increase sensitivity within sleep, mood, and cognitive systems.
For some women, menopausal hormone therapy (MHT) may be considered as part of management following careful individual assessment. International guidance recognises that addressing vasomotor symptoms may improve sleep and quality of life for some women.
However:
- Hormones are rarely the only factor
- Hormonal therapy is not appropriate for everyone
- Benefits and risks must be considered individually
Hormonal therapy, where appropriate, is typically part of a broader management plan rather than a standalone solution.
Non-hormonal medical options
For women who are unable or prefer not to use hormone-based therapies, evidence-based non-hormonal options may be considered.
These may be used to support:
- Vasomotor symptoms
- Sleep disruption
- Mood or anxiety symptoms
International menopause guidance recognises non-hormonal therapies as valid options when clinically appropriate.
Supporting mood, anxiety, and cognitive symptoms
Where anxiety, low mood, or cognitive symptoms are prominent, management may involve:
- Addressing sleep disruption
- Psychological or behavioural therapies
- Reviewing contributing medical factors
- Considering broader mental health supports where indicated
Distinguishing menopausal vulnerability from primary mental health conditions is an important part of assessment.
The importance of individualised care
Effective menopause care does not focus on a single symptom or system in isolation.
A structured approach considers:
- Symptom patterns and severity
- Sleep quality
- Hormonal stage and symptoms
- Physical and mental health history
- Lifestyle context and stressors
- Individual preferences and goals
This whole-picture approach is supported by current clinical guidance and reflects how menopause care is delivered in practice.
Key takeaway
Sleep disturbance, mood changes, anxiety, and cognitive symptoms during perimenopause and menopause are common, interconnected, and highly individual.
Evidence supports a stepwise, personalised approach that may include behavioural strategies, psychological therapies, hormonal and non-hormonal options, and lifestyle support — selected according to individual needs and circumstances.
If you would like to seek further information about these symptoms or learn more about assessment options, you can contact Menopause & Me:
🌐 menopauseandme.com.au/booking
You’re not alone on this journey: knowledge is power!
Warm Regards,
Jenna Bell
Nurse Practitioner & Menopause Educator
Sources
Australasian Menopause Society | International Menopause Society | North American Menopause Society | NICE Guidelines NG23
Important Disclaimer: The information in this blog/newsletter is general in nature and intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your Nurse Practitioner, doctor, or another qualified health practitioner with any questions you may have regarding a medical condition or before commencing any new treatment, exercise program, changing your diet, or taking supplements – particularly if you have existing health conditions, are on medication, or have had fractures or falls in the past. Individual needs and responses vary.
Sleep, Mood, Anxiety & Brain Fog: Understanding the Overlap in Perimenopause and Menopause [Menopause Symptoms & Systems Series (Part 2 of 3)]
Hello and welcome to Menopause & Me.
In Part 1 of this series, we explored why sleep and fatigue commonly change during perimenopause and menopause, and why sleep disturbance at this stage is often multifactorial rather than hormone-driven alone.
In Part 2, we look at why sleep disturbance, low mood, anxiety, and cognitive symptoms such as “brain fog” so often occur together during the menopause transition — and why these experiences are best understood as interconnected systems rather than isolated symptoms. (click on the arrow to the left to open the full article)
Why these symptoms often occur together
Many women are surprised to experience new or worsening anxiety, low mood, irritability, or cognitive changes during perimenopause — particularly if they have never had mental health concerns before.
Sleep, mood, anxiety, and cognition are closely linked through shared brain pathways and neurochemical systems. Changes in one area can influence the others, creating a bidirectional cycle:
- Poor sleep can worsen mood, anxiety, and concentration
- Anxiety and low mood can disrupt sleep initiation and maintenance
- Cognitive symptoms may be amplified by fatigue, stress, and fragmented sleep
Understanding this overlap helps explain why symptoms may feel broad, unpredictable, or disproportionate to a single cause.
Hormonal influences on the brain (high-level overview)
Oestrogen and progesterone influence several neurotransmitter systems involved in emotional regulation, stress response, and cognitive processing, including serotonin, GABA, and dopamine.
During the menopause transition, fluctuating or declining hormone levels may increase sensitivity within these systems. This does not mean hormones are the sole cause of mood or cognitive symptoms, but rather that the brain may become more vulnerable to stressors that were previously well tolerated.
Importantly, this vulnerability varies widely between individuals.
The sleep–mood–stress connection
Sleep disturbance is both a symptom and a driver of emotional and cognitive change.
Fragmented or insufficient sleep can:
- Lower stress tolerance
- Increase emotional reactivity
- Reduce concentration and memory efficiency
- Exacerbate anxiety and low mood
At the same time, heightened stress, worry, or mood changes can make it harder to fall asleep or stay asleep, reinforcing the cycle.
This overlap explains why addressing sleep patterns is often a key component of broader symptom assessment in perimenopause and menopause.
Understanding “brain fog”
“Brain fog” is a commonly reported term used to describe experiences such as:
- Reduced concentration or focus
- Slower word retrieval
- Forgetfulness
- Feeling mentally less sharp or efficient
In midlife women, these symptoms are often functional rather than degenerative. They may reflect the combined effects of sleep disruption, stress, hormonal sensitivity, and cognitive load, rather than underlying neurological disease.
While frustrating, these changes are typically subtle, fluctuate over time, and are not associated with progressive cognitive decline.
Anxiety and mood changes in midlife
Some women experience:
- New-onset anxiety
- Increased worry or rumination
- Panic symptoms
- Low mood or loss of enjoyment
- Heightened emotional sensitivity
These changes may occur even in women with no prior mental health history. For others, existing anxiety or mood disorders may worsen during the menopause transition.
Distinguishing between menopausal vulnerability, situational stressors, sleep-related effects, and primary mental health conditions is an important part of clinical assessment.
Other contributing factors to consider
As with sleep disturbance, mood and cognitive symptoms should not automatically be attributed to menopause alone. Other contributors may include:
- Chronic stress or burnout
- Caring responsibilities or life transitions
- Thyroid dysfunction
- Iron deficiency
- Medication effects
- Alcohol sensitivity
- Underlying mental health conditions
A systems-based approach helps ensure important contributors are not overlooked.
When to consider a clinical review
A longer or more comprehensive review may be appropriate if mood, anxiety, or cognitive symptoms:
- Are persistent or worsening over time
- Interfere with work, relationships, or daily functioning
- Are associated with significant sleep disruption
- Include panic symptoms or marked distress
- Are accompanied by physical symptoms such as palpitations, tremor, or unexplained weight change
- Raise concerns about safety or wellbeing
Assessment may involve exploring symptom patterns, sleep quality, medical history, psychosocial factors, and, where appropriate, further investigation.
Key takeaway
Sleep disturbance, mood changes, anxiety, and cognitive symptoms commonly overlap during perimenopause and menopause. These experiences are best understood as interconnected systems influenced by hormonal sensitivity, sleep quality, stress, and individual context.
A structured, individualised approach, rather than focusing on a single symptom in isolation, is supported by current clinical guidance.
In Part 3, we will explore how clinicians think about evidence-based management pathways, including hormonal and non-hormonal options, sleep-focused strategies, and broader supportive approaches.
If you would like to seek further information about these symptoms or learn more about assessment options, you can contact Menopause & Me:
🌐 menopauseandme.com.au/booking
You’re not alone on this journey: knowledge is power!
Warm Regards,
Jenna Bell
Nurse Practitioner & Menopause Educator
P.S. Missed our recent editions?
They’re all saved on the website for you anytime in the blog section
Sources
Australasian Menopause Society | International Menopause Society | North American Menopause Society | NICE Guidelines NG23
Important Disclaimer: The information in this blog/newsletter is general in nature and intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your Nurse Practitioner, doctor, or another qualified health practitioner with any questions you may have regarding a medical condition or before commencing any new treatment, exercise program, changing your diet, or taking supplements – particularly if you have existing health conditions, are on medication, or have had fractures or falls in the past. Individual needs and responses vary.
Sleep & Fatigue: Understanding Sleep Changes in Perimenopause and Menopause [Menopause Symptoms & Systems Series (Part 1 of 3)]
Hello and welcome to the Menopause & Me community,
Changes to sleep and persistent fatigue are among the most commonly reported concerns during perimenopause and menopause. Many women describe lighter sleep, frequent waking, early morning waking, or feeling unrefreshed despite adequate time in bed.
Sleep disturbance during this life stage is often multifactorial. While hormonal changes and vasomotor symptoms may contribute significantly, they are rarely the only factors. A thorough understanding of possible contributors supports appropriate, individualised assessment and management. (click on the arrow to the left to open the full article)
Why sleep can change during perimenopause and menopause?

Vasomotor symptoms and sleep disruption
Hot flushes and night sweats can fragment sleep, trigger waking episodes, and reduce overall sleep quality. For some women, effectively addressing vasomotor symptoms may improve subjective sleep quality.
However, not all sleep disturbance during menopause is driven by vasomotor symptoms alone.
Hormonal influence on sleep regulation
Oestrogen and progesterone interact with brain pathways involved in thermoregulation, mood, and sleep–wake regulation. During the menopause transition, fluctuating or declining hormone levels may increase vulnerability to sleep disruption, even in the absence of other health changes.
Importantly, hormonal change is rarely the sole cause of sleep disturbance.
Other contributors common in midlife
Sleep changes during this stage may also be influenced by:
- Sleep apnoea or snoring
- Iron deficiency or restless legs symptoms
- Thyroid dysfunction
- Anxiety or low mood
- Increased sensitivity to alcohol
- Caring responsibilities, work demands, or chronic stress
For this reason, sleep disruption should not automatically be attributed to menopause alone, and other contributing factors may need to be considered and addressed.
How sleep disturbance may present
Women may notice:
- Difficulty falling asleep
- Frequent night-time waking
- Early morning waking with difficulty returning to sleep
- Non-restorative sleep
- Daytime fatigue, reduced concentration, or irritability
While these experiences are common, they are not insignificant and warrant assessment if they persist or interfere with daily functioning.

An evidence-based approach to assessment
Step 1: Identify your sleep pattern
Tracking sleep for 1–2 weeks can be helpful. This may include:
- Bedtime and wake time
- Night sweats (if present)
- Alcohol or caffeine intake
- Exercise timing
- Mood or stress levels
- Duration and frequency of night waking
Identifying patterns can help differentiate between insomnia, vasomotor-related sleep disruption, circadian rhythm changes, or other sleep disorders.
Step 2: Consider insomnia-focused approaches when appropriate
For women experiencing persistent insomnia, cognitive behavioural therapy for insomnia (CBT-I) is recognised as a first-line, evidence-based management option.
CBT-I is a structured, non-medication therapy that focuses on how sleep habits, behaviours, and thought patterns influence sleep quality. It commonly includes strategies such as:
- Improving sleep consistency and sleep drive
- Reducing behaviours that unintentionally disrupt sleep
- Addressing unhelpful beliefs or anxiety related to sleep
International guidance, including NICE Guideline NG23 (updated 7 November 2024), supports menopause-specific CBT approaches for sleep difficulties associated with vasomotor symptoms, as well as broader cognitive and behavioural strategies for menopause-related sleep disturbance.
Recent research continues to support the role of CBT-I in this population.
Step 3: Address contributing symptoms
Where vasomotor symptoms are a major contributor to sleep disruption, symptom-directed approaches may be considered following individual clinical assessment.
For women who are unable or prefer not to use hormone-based therapies, non-hormonal options — supported by evidence such as the NAMS Nonhormone Therapy Position Statement — may also be discussed where appropriate.
Practical strategies that may support sleep
The following approaches may be helpful, depending on the underlying pattern and are aligned with lifestyle guidance from menopause societies such as the Australasian Menopause Society, which emphasise restorative sleep as part of midlife health:
If night sweats are present
- Maintaining a cool bedroom environment
- Using breathable bedding and layered sleepwear
- Limiting alcohol and heavy meals close to bedtime
If difficulty settling or racing thoughts occur
- Establishing a consistent wind-down routine
- Limiting stimulating activities before bed
- Structured insomnia-focused strategies (such as CBT-I principles)
If early morning waking is a concern
- Keeping wake times consistent
- Exposure to morning daylight
- Avoiding long or late naps
When to consider a clinical review
A longer appointment may be appropriate if sleep disturbance:
- Persists most nights for more than four weeks
- Is associated with loud snoring, gasping, or marked daytime sleepiness
- Occurs alongside persistent low mood or anxiety
- Is accompanied by symptoms such as restless legs, palpitations, or unexplained weight change
- Is associated with bleeding changes or other new health concerns
Assessment may involve reviewing symptoms, medical history, medications, and, where appropriate, further investigation.
Key takeaway
Sleep and fatigue changes during perimenopause and menopause are common and often multifactorial. A structured, individualised approach — identifying contributing factors and tailoring assessment and management accordingly — is strongly supported by current clinical guidance.
If you would like to seek further information about sleep changes during menopause, or learn more about available assessment options, you can contact Menopause & Me:
🌐 menopauseandme.com.au/booking
You’re not alone on this journey: knowledge is power!
Warm Regards,
Jenna Bell
Nurse Practitioner & Menopause Educator
P.S. Missed our recent editions?
They’re all saved on the website for you anytime in the blog section
Sources
Australasian Menopause Society | International Menopause Society | North American Menopause Society | NICE Guidelines NG23
Important Disclaimer: The information in this blog/newsletter is general in nature and intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your Nurse Practitioner, doctor, or another qualified health practitioner with any questions you may have regarding a medical condition or before commencing any new treatment, exercise program, changing your diet, or taking supplements – particularly if you have existing health conditions, are on medication, or have had fractures or falls in the past. Individual needs and responses vary.
Skin & Hair Changes in Menopause: Understanding What’s Happening and How to Support Healthy Ageing
Hello and welcome to the Menopause & Me community,
Menopause and the years leading up to it can bring noticeable changes to skin and hair. Many women report dryness, changes in texture, thinning hair, or differences in how their skin responds to products that once worked well.
These changes are common and biologically driven. This newsletter explains why they occur and outlines evidence-based ways to support skin and hair health during midlife. (click on the arrow to the left to open the full article)
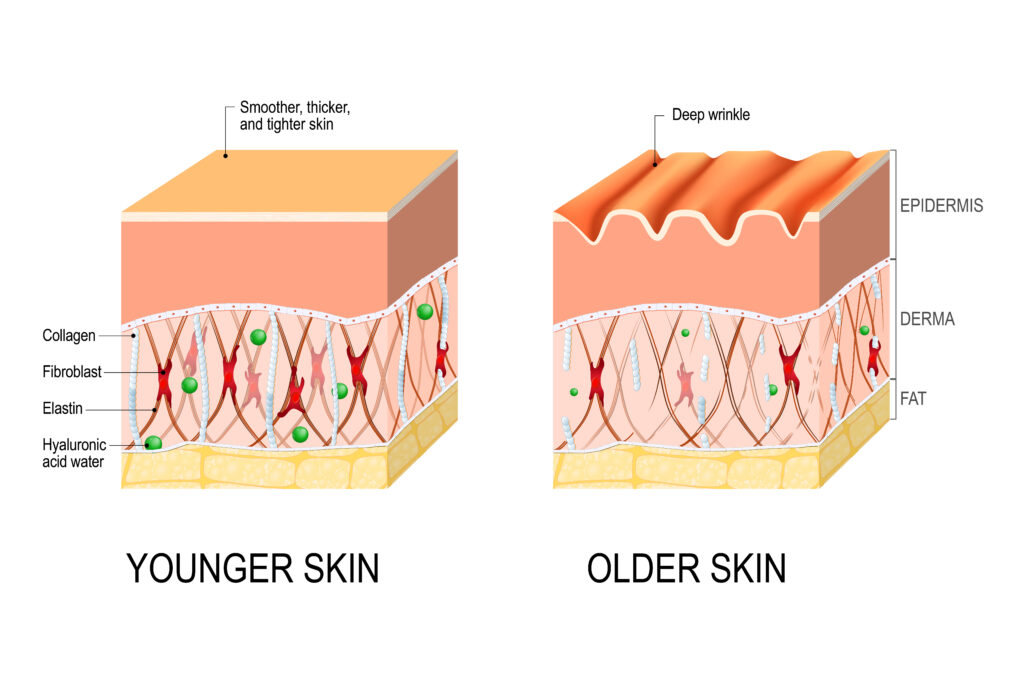
Why Skin Changes Occur in Menopause
Oestrogen plays an important role in maintaining skin structure and function. As levels decline during perimenopause and menopause, several changes can occur:
- Reduced collagen production and accelerated collagen breakdown
- Decreased skin thickness and elasticity
- Reduced natural oils and hydration
- Impaired skin barrier function
Research suggests that up to 30 percent of skin collagen may be lost within the first five years after menopause, with ongoing gradual decline thereafter.
Common skin changes reported include:
- Dryness, itching, or increased sensitivity
- Fine lines and deeper wrinkles
- Loss of firmness or sagging
- Changes in pigmentation or uneven tone
- Adult-onset or persistent acne related to hormonal fluctuation

Why Hair Changes Occur in Menopause
Hair growth is influenced by hormonal balance. As oestrogen and progesterone levels fall:
- The active (growth) phase of the hair cycle shortens
- Hair follicles may become smaller over time
- Relative androgen activity may increase
As a result, many women notice:
- Diffuse thinning or widening of the part (female-pattern hair thinning)
- Dry, brittle hair texture
- Slower regrowth
- Increased facial hair in some areas

Evidence-Based Ways to Support Skin and Hair Health
Lifestyle and topical care remain first-line strategies:
- Use gentle cleansers and moisturisers containing ceramides or hyaluronic acid
- Apply broad-spectrum sunscreen daily
- Introduce retinoids or peptides gradually if appropriate
- Ensure adequate dietary protein, essential fats, and antioxidants
- Prioritise sleep and stress management
Hormone therapy:
For women who are suitable candidates, menopause hormone therapy has been shown to improve skin hydration, elasticity, and collagen content. Evidence for direct benefits on scalp hair is more limited and outcomes vary between individuals.
A Simple 3-Step Approach
- Observe and track changes
Photos or brief journaling can help identify patterns over time. - Seek a clinical review
Other contributors such as iron deficiency, thyroid conditions, nutritional gaps, or dermatological conditions should be considered. - Ask targeted questions
“Which skincare, hair treatments, or medical options are appropriate for me?”
If you’d like support or a personalised plan, you can reach me at:
📧 hello@menopauseandme.com.au
🌐 menopauseandme.com.au
Warmly,
Jenna
Nurse Practitioner & Menopause Educator
Sources
Australasian Menopause Society | North American Menopause Society | International Menopause Society | European Menopause and Andropause Society | Brincat M et al. Skin ageing and menopause. Climacteric | Thornton MJ. Oestrogen and hair follicle biology. Journal of Endocrinology | Affinito P et al. Effects of hormone therapy on skin collagen. Maturitas
Important Disclaimer: The information in this blog/newsletter is general in nature and intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your Nurse Practitioner, doctor, or another qualified health practitioner with any questions you may have regarding a medical condition or before commencing any new treatment, exercise program, changing your diet, or taking supplements – particularly if you have existing health conditions, are on medication, or have had fractures or falls in the past. Individual needs and responses vary.
Progesterone, Testosterone & DHEA: The Supporting Cast (Part 3 of 3)
This is the final part of our hormone series. Today we look at three hormones that can play a role for some women when clinically indicated: progesterone, testosterone, and DHEA (prasterone). These may be used alongside oestradiol in menopause care, depending on your symptoms, medical history, and goals. (click on the arrow to the left to open the full article)
Progesterone recap
Progesterone receptors are found in many tissues (including the uterus and brain). In menopause hormone therapy (MHT), progesterone (or another progestogen) is primarily used to protect the lining of the uterus (endometrium) when oestrogen is prescribed and you still have a uterus.
Some women also report improvements in sleep or mood with certain progestogens, but responses vary and this isn’t the main reason progesterone is prescribed in MHT.
Body-identical option:
- Micronised progesterone (e.g., Utrogestan) is the body-identical progesterone option used in MHT.
Common TGA-approved progesterone options in Australia
- Micronised progesterone capsules (e.g., Utrogestan): used orally for MHT and also used vaginally in some contexts (follow prescriber advice and product information).
- Other progestogens may be used for endometrial protection depending on the regimen and individual factors (your clinician will guide this).
Key safety point: If you have a uterus and are using systemic oestrogen for MHT, a progestogen is usually required to reduce the risk of endometrial hyperplasia/cancer.
Testosterone recap
Women produce testosterone across the lifespan, and it plays a role in sexual function among other physiological processes. However, when it comes to menopause care, international consensus is clear:
The only evidence-based indication for systemic testosterone therapy in women is:
✅ Hypoactive Sexual Desire Disorder (HSDD) in postmenopausal women, after a biopsychosocial assessment and after other contributing factors are addressed.
There is insufficient evidence to recommend testosterone for problems such as fatigue, “brain fog”, mood, or disease prevention.
TGA-approved option in Australia
- AndroFeme 1 (testosterone cream) is TGA-registered for HSDD in postmenopausal women.
PBS note (important correction):
- As of December 2025, AndroFeme 1 is not PBS-listed, following a PBAC decision not to recommend listing.
Monitoring matters: If testosterone is prescribed, guidelines recommend using the lowest effective dose, aiming for physiological female ranges, and monitoring for side effects (e.g., acne, hair changes) and blood levels.
DHEA recap (prasterone)
DHEA is an adrenal precursor hormone that declines with age. In menopause care, the most established role is local vaginal DHEA (prasterone) for symptoms of genitourinary syndrome of menopause (GSM) such as dryness and painful sex.
TGA-approved option in Australia
- Intrarosa (prasterone) vaginal pessaries are TGA-approved for moderate–severe vulvar and vaginal atrophy in postmenopausal women. Therapeutic Goods Administration (TGA)+1
Important safety note (correction):
- Australian prescribing information and Australian Prescriber reporting indicate contraindications, including a history of breast cancer or thromboembolism. This is a situation where personalised specialist advice is essential. Australian Prescriber+1
Oral DHEA supplements:
- Evidence for broad menopause symptom relief is limited and inconsistent, and they’re not routinely recommended in major menopause guidance. menopause.org.au+1
What symptom changes are realistic?
Guidelines support the following, when therapy is clinically indicated:
- Progesterone (as part of MHT if you have a uterus): endometrial protection; some women notice sleep benefits, but this varies.
- Testosterone (for diagnosed HSDD): can improve sexual desire and related distress in postmenopausal women; effects are typically moderate.
- Vaginal DHEA (prasterone): can improve vaginal tissue symptoms and painful sex related to GSM.
Individual responses vary, and treatment choice depends on your overall health and preferences.
Your helpful 3-step plan
- Reflect on symptoms
- Uterus + systemic oestrogen? You’ll usually need a progestogen for uterine protection. menopause.org.au+1
- Distressing low desire? Ask whether assessment for HSDD is appropriate. International Menopause Society+1
- Vaginal dryness/pain? Ask about local GSM treatments (vaginal oestrogen, prasterone, other options). Dutch Menopause Society+1
- Book with a menopause-trained health professional
- Ask: “Are progesterone, testosterone or vaginal DHEA options for my needs—and what monitoring would be required?”
Non-hormonal supports that still matter
- Resistance training 2–3 times/week supports strength, function, and bone health across midlife. Monash University+1
- Sleep and stress supports (routine, light exposure, limiting alcohol, addressing sleep disorders) can improve wellbeing alongside medical care. Monash University+1
- Protein-rich meals and adequate overall nutrition support muscle and energy. Monash University+1
If you’ve missed the first two newsletters in this series, you can find them — along with all previous newsletters — at menopauseandme.com.au/blog.
If you’d like support or a personalised plan, you can reach me at:
📧 hello@menopauseandme.com.au
🌐 menopauseandme.com.au/booking
Warmly,
Jenna
Nurse Practitioner & Menopause Educator
Sources
Australasian Menopause Society (AMS) – Treatment options & MHT dosing resources
The Menopause Society (NAMS) – 2022 Hormone Therapy Position Statement
International Menopause Society (IMS) – Global Consensus on Testosterone Therapy for Women (2019)
Jean Hailes for Women’s Health – Menopausal hormone therapy & testosterone guidance
Monash University – Practitioner’s Toolkit for Managing Menopause (updated 2025)
TGA (Australia) – Intrarosa (prasterone) + ARTG listing
NPS MedicineWise – AndroFeme 1 (indication and consumer information)
Australian Prescriber – Prasterone overview and contraindications
Important Disclaimer: The information in this blog/newsletter is general in nature and intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your Nurse Practitioner, doctor, or another qualified health practitioner with any questions you may have regarding a medical condition or before commencing any new treatment, exercise program, changing your diet, or taking supplements – particularly if you have existing health conditions, are on medication, or have had fractures or falls in the past. Individual needs and responses vary.
Oestrogen Essentials: Options to Ease Symptoms & Protect Long-Term Health (Part 2 of 3)
In Part 1, we explored how sex hormones work together to influence your whole body. Today, we zoom in on oestradiol — the hormone that drives many of the changes women notice through perimenopause and menopause.
Building on Part 1, this week we focus on oestradiol: the most potent oestrogen and the one that declines most dramatically in menopause. It plays a role in hot flushes, sleep, mood, joint comfort, bladder health, sexual comfort, brain function, bone strength, cardiovascular health and skin integrity. (click on the arrow to the left to open the full article)
Oestrogen Recap
Oestrogen receptors are found body-wide (quick visual reminder):
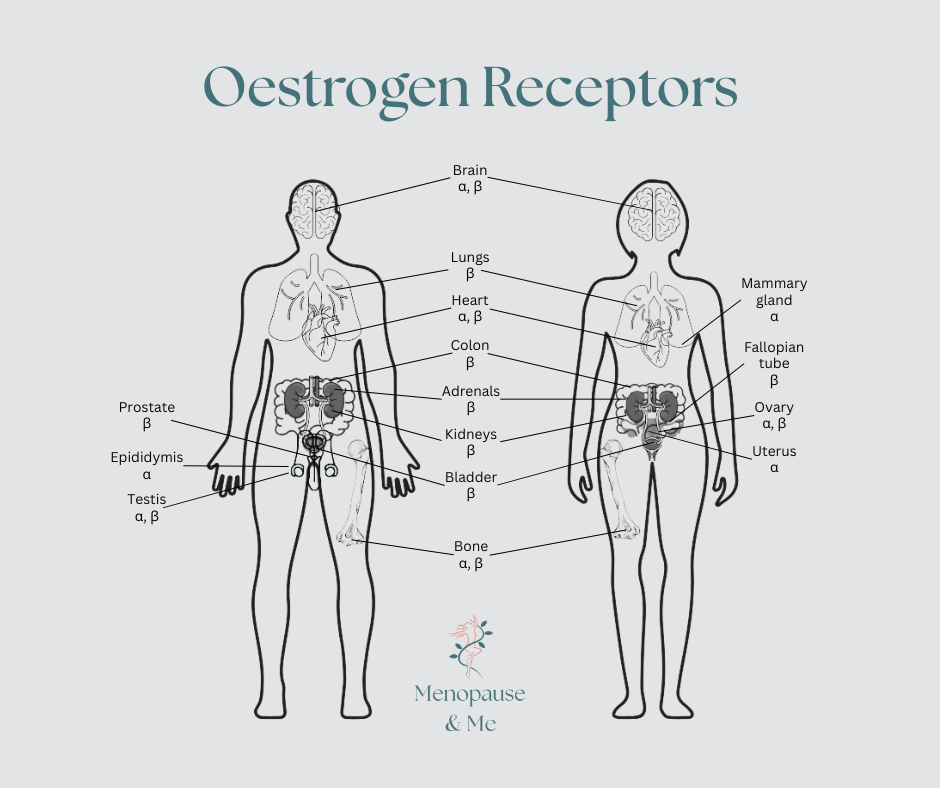
Adapted from tissue distribution data in Paterni et al. (2014) Steroids and Australasian Menopause Society guidelines (2025). Illustration by Menopause & Me.
Brain • Heart and blood vessels • Bones and muscles • Skin and collagen • Bladder and vagina • Many more
- Oestradiol (E2): The strongest and most active before menopause. Produced mainly by the ovaries. This is the key oestrogen in menopause hormone therapy.
- Oestrone (E1): Weaker than oestradiol. Becomes the main oestrogen after menopause (produced in fat tissue).
- Oestriol (E3): The weakest. Mainly produced during pregnancy by the placenta.
- Oestetrol (E4): Produced only during pregnancy by the fetal liver.
In menopause therapy, we primarily replace oestradiol because it most closely matches what your body made in higher amounts pre-menopause.
Safe, TGA-approved oestrogen options in Australia (2025)
Transdermal routes (patches/gels) generally have the lowest risk profile.
| Route | Common examples | Clot risk (standard doses) | Often suitable for |
| Transdermal patch | Estradot, Climara | Not associated with increased VTE risk in most guideline summaries at standard doses | Most women, including higher-risk profiles |
| Transdermal gel | Estrogel, Sandrena | Not associated with increased VTE risk in most guideline summaries at standard doses | Flexible dosing |
| Oral tablets | Progynova, Zumenon | Associated with a small increase in VTE risk compared with transdermal routes | Convenience (if no clot concerns) |
| Vaginal (local) | Vagifem pessaries, Ovestin cream | Minimal systemic absorption; VTE risk not increased | Genitourinary symptoms only |
Many are PBS-subsidised.
Common symptom relief (from guidelines)
Many women notice:
- Clinical trials show substantial reductions (often in the range of 75-90%) in hot flushes for many women
- Improvement in vaginal dryness, painful sex and bladder symptoms
- Better sleep, mood and joint comfort
- Reduced brain fog
Individual responses vary.
Long-term considerations (when started early: under 60 or within 10 years of menopause)
Guidelines note potential benefits including:
- Reduced bone loss and fractures
- Neutral to potentially beneficial cardiovascular effects have been observed when started early, particularly with transdermal formulations
At standard doses, risks are considered low in guideline summaries, but decisions are always individualised.
Your helpful 3-step plan
- Continue tracking symptoms
- Book a longer appointment with your clinician
- Ask: “Is oestradiol a safe option for my history and symptoms?”

Non-hormonal helpers that make a real difference
Many women start here for mild to moderate symptoms:
- Keep core body temperature lower (layered bedding, cool room, fans, cold drinks)
- Identify and reduce personal triggers (caffeine, alcohol, spicy foods)
- Practice paced breathing or relaxation during a flush
- Regular physical activity (e.g., walking, yoga or strength training 2–3 times/week)
- Maintain a healthy weight (evidence shows weight gain can worsen flushes)
- Cognitive behavioural therapy (CBT) or clinical hypnosis (some evidence for reducing flush bother and improving sleep/mood)
Next up: Part 3 (Progesterone, Testosterone and DHEA).
If you’d like support or a personalised plan, you can reach me at:
🌐 menopauseandme.com.au/booking
You’re not alone on this journey: knowledge is power!
Warmly, Jenna
Nurse Practitioner
Sources
Australasian Menopause Society | North American Menopause Society Position Statement | Jean Hailes for Women’s Health | Monash University Practitioner Toolkit
Important Disclaimer: The information in this blog/newsletter is general in nature and intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your Nurse Practitioner, doctor, or another qualified health practitioner with any questions you may have regarding a medical condition or before commencing any new treatment, exercise program, changing your diet, or taking supplements – particularly if you have existing health conditions, are on medication, or have had fractures or falls in the past. Individual needs and responses vary.
Sex Hormones 101: How They Keep You Thriving Through Change (Part 1 of 3)
Welcome to a brand-new 3-part series exploring the incredible role sex hormones play in your mood, energy, bones, heart, brain, skin, bladder — literally everything! (click on the arrow to the left to open the full article)
What are sex hormones, really?
They’re powerful chemical messengers made from cholesterol that coordinate functions across your entire body. Women and men have the same three main sex hormones — just in different amounts and patterns throughout life:
- Oestradiol (the most potent oestrogen – your pre-menopause superstar)
- Progesterone (the calming balancer)
- Testosterone (supports energy, libido, muscle and bone strength)
These hormones don’t just affect reproduction — their receptors are found throughout your body:
Brain (mood, memory, sleep) • Heart & blood vessels • Bones & muscles • Skin & hair •Eyes & saliva glands • Bladder & vagina • Gut • Mitochondria (cell energy factories)
Common symptoms linked to these changes
Symptoms vary hugely woman to woman, but here are some of the most reported:
Physical
- Hot flushes & night sweats
- Joint or muscle aches
- Fatigue & low energy
- Thinning hair or dry skin
- Weight changes (especially around middle)
Genitourinary (vaginal, sexual & bladder)
- Vaginal dryness & painful sex
- Urinary urgency, frequency or recurrent UTIs
Emotional & cognitive
- Low mood, anxiety or irritability
- Brain fog & memory lapses
- Sleep disturbance
- Reduced libido
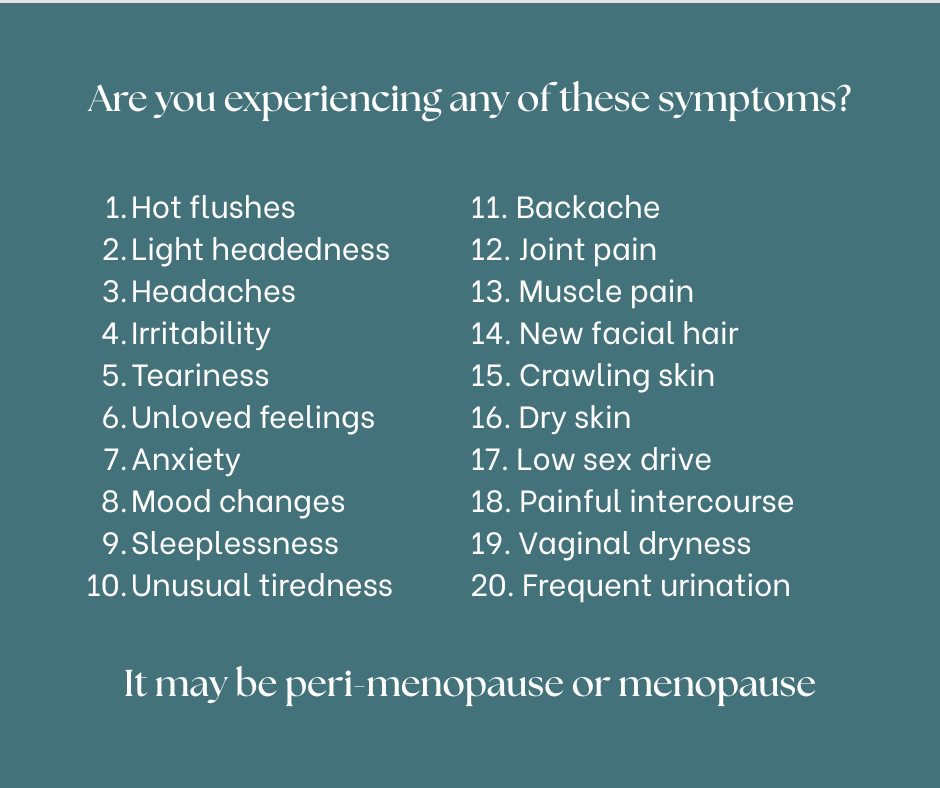
Remember: A wide range of symptoms may be influenced by perimenopause or menopause… but it’s essential to rule out other causes first with your clinician.
Your helpful 3-step starting point
- Track your symptoms for 2–4 weeks (frequency, severity, triggers)
- Book a longer appointment with your Nurse Practitioner
- Take your tracker and ask: “Could changing hormones be contributing?”

Non-hormonal helpers that make a real difference
- Paced breathing or mindfulness during hot flushes
- Regular movement (walking, yoga, strength training 2× week)
- Cool bedroom, cotton sheets & layered bedding
- Reducing personal triggers (caffeine, alcohol, spicy foods)
- Prioritising protein & calcium-rich foods
Next up – Part 2: Estrogen Essentials (safe options, symptom relief & long-term
protection).
You’re not alone on this journey — knowledge is power!
If you’d like support or a personalised plan, you can reach me at:
📧 hello@menopauseandme.com.au
🌐menopauseandme.com.au/booking
Warmly,
Jenna
Nurse Practitioner & Menopause Educator
Sources
Australasian Menopause Society | North American Menopause Society Position Statement | Jean Hailes for Women’s Health | Monash University Practitioner Toolkit
Important Disclaimer: The information in this blog/newsletter is general in nature and intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your Nurse Practitioner, doctor, or another qualified health practitioner with any questions you may have regarding a medical condition or before commencing any new treatment, exercise program, changing your diet, or taking supplements – particularly if you have existing health conditions, are on medication, or have had fractures or falls in the past. Individual needs and responses vary.
Bioidentical Hormones: Understanding Your Options in Perimenopause & Menopause
If you’re experiencing changes in sleep, mood, energy, hot flushes, or discomfort during sex, you’re certainly not alone. These changes are common during perimenopause and menopause, and there are several evidence-based options that may support you through this transition.
I’m Jenna, your Nurse Practitioner and menopause educator. This guide helps make sense of the different hormone therapy options available in Australia, how they work, and how to approach treatment in a way that’s safe, informed and tailored to you. (click on the arrow to the left to open the full article)
What does “bioidentical” actually mean?
Bioidentical hormones have the same molecular structure as the hormones your ovaries produced before menopause. These include:
- Oestradiol (the main form of oestrogen)
- Micronised progesterone
- Physiologic-dose testosterone (for specific indications)
In Australia, bioidentical hormones are available in two forms:
✔ TGA-approved bioidentical products
These are standardised, regulated medicines (patches, gels, capsules, tablets).
✔ Compounded bioidentical hormones*
These may be considered when:
- a person cannot tolerate TGA-approved products
- they require an excipient-free option
- a specific dose or formulation is needed that is not commercially available
Because compounded products are not TGA-approved and may vary in strength and purity, they are not first-line in Australian and international guidelines.
However, they can be appropriate in selected cases following an individualised discussion of risks, benefits and alternatives.
This means compounded options remain available — just not the default starting point.
*Always discuss risks like inconsistent dosing/purity with your practitioner
Bioidentical, Synthetic and Compounded Hormones – Understanding the Differences
Both synthetic and bioidentical hormones have been used safely for decades and are supported by substantial international research. The best choice depends on symptoms, health history, preferences and individual tolerability.
Below is a simple, AHPRA-compliant comparison of key characteristics, not expected outcomes.
📊 Key Characteristics of Hormone Therapy Options
(AMS, NAMS, NICE, Monash Toolkit — 2024–2025)
Individual suitability varies; outcomes are not guaranteed.
| Category | TGA-Approved Bioidentical Oestradiol & Micronised Progesterone | Synthetic Oestrogens & Progestins | Compounded Bioidentical Hormones |
| Structure | Identical to human hormones. | Different molecular structure. | Identical to human hormones. |
| Regulation | TGA-approved, standardised and quality-controlled. | TGA-approved, standardised and quality-controlled. | Not TGA-approved; quality and strength may vary. |
| Metabolism | Processed similarly to natural hormones. | Metabolised differently depending on the type. | Similar to bioidentical hormones, but consistency varies. |
| Routes Available | Patches, gels, capsules, tablets. | Tablets, some patches. | Custom routes (e.g., troches, creams) if clinically required. |
| VTE/Clot Considerations | Transdermal oestradiol is not associated with increased clot risk in most guideline summaries. | Oral oestrogens are associated with increased clot risk compared with transdermal routes. | Depends on formulation and route; evidence is limited. |
| Progesterone Tolerability | Micronised progesterone is often described as well-tolerated in guideline summaries. | Tolerability varies; some progestins may affect mood for some individuals. | May assist people who cannot tolerate approved products; evidence is limited. |
| Sleep & Mood | Some women report improved sleep with micronised progesterone. Responses vary. | Varies widely by individual and formulation. | Varies; limited evidence. |
| Metabolic Effects | Transdermal oestradiol tends not to significantly affect blood pressure or lipids. | Some oral formulations may influence lipids or blood pressure. | Unknown; dependent on compound and route. |
| Guideline Position | Commonly recommended first-line when using transdermal oestradiol + micronised progesterone. | Safe and appropriate for many women. | Considered when approved options are unsuitable. |
Treatment Options in Australia
Depending on your symptoms and where you are in the menopause transition, options may include:
- Oestradiol (gel, patch or tablet)
- Micronised progesterone
- Combined oestrogen–progestin tablets
- Low-dose vaginal oestrogen for dryness and discomfort
- Testosterone for low sexual desire when clinically indicated
Suitability varies from person to person. Age, medical history, personal risk factors and prior responses to treatment all help guide decision-making.
A simple way to explore your options
Here’s a supportive way to begin:
- Track your symptoms for 2–4 weeks.
- Book a longer consultation to allow time for discussion.
- Bring this newsletter and ask:
“Which option aligns best with my health history and goals?”
Hormone therapy often requires minor adjustments over time to find the right fit.
Non-hormonal choices
Some women prefer non-hormonal options or cannot use hormones. Evidence-based alternatives include:
- Non-hormonal medications for hot flushes
- Cognitive behavioural strategies for flushes and sleep
- Regular vaginal moisturisers and lubricants
- Strength training, movement and sleep optimisation
- Tracking and reducing personal triggers such as alcohol or caffeine
You’re supported
Perimenopause and menopause are significant life phases. With personalised care, many women find approaches that help improve comfort, confidence and daily wellbeing.
If you’d like support or a personalised plan, you can reach me at:
📧 hello@menopauseandme.com.au
🌐 menopauseandme.com.au
Warmly,
Jenna
Nurse Practitioner & Menopause Educator
Sources (2024–2025)
Australasian Menopause Society (AMS)
NICE NG23
North American Menopause Society (NAMS)
Monash University Practitioner Toolkit
Jean Hailes for Women’s Health
Therapeutic Goods Administration (TGA)
Medical Disclaimer
This newsletter contains general information only and does not replace personalised medical advice. Hormone therapy is not suitable for everyone. All treatment decisions should be made in consultation with a qualified health professional.
Building Strong Foundations: Weight Training, Protein, and Bone Health in Perimenopause, Menopause, and Beyond
If you’ve felt the subtle (or not-so-subtle) shifts in your body during perimenopause—like that extra ache in your joints or a sneaky dip in energy—you’re spot on that it’s time to talk strength.
As we navigate these stages, our bones and muscles need extra TLC, especially with osteoporosis lurking as a silent risk. But here’s the uplifting Aussie truth: incorporating weight training and smart protein intake isn’t just about prevention—it’s a game-changer for vitality, confidence, and long-term health.
Drawing from trusted local guidelines, this edition unpacks the why, the how, and the hope, so you can lift your way to a stronger you. Whether you’re in the thick of perimenopause flushes or settling into post-menopause freedom, let’s build resilience together. (click on the arrow to the left to open the full article)
The Hidden Risk: Osteoporosis in Midlife and Beyond
Menopause marks a pivotal shift for bone health, thanks to plummeting oestrogen levels that once protected your skeleton. In perimenopause, fluctuations start the subtle erosion; by menopause (average age 51 in Australia), bone loss accelerates, and post-menopause, it becomes a steady concern—potentially spanning decades.
Osteoporosis, or “brittle bones,” affects an estimated 23% of Aussie women over 50, making fractures from simple falls a real threat (think hip, spine, or wrist). Around 42% of Australian women over 50 face a lifetime risk of an osteoporosis-related fracture—most from a simple fall from standing height. Post-menopause, oestrogen’s absence means bones break down faster than they rebuild, with women losing up to 2% density annually in the first few years.
Risks spike if you smoke, drink heavily, or have a family history, but even without those, the hormonal drop puts us all in the spotlight. The good news? Early action—like the strategies below—can slash fracture risk by up to 50%, per Healthy Bones Australia.
Why Weight Training is Your Menopause Superpower ?
Enter resistance training (think weights, bands, or bodyweight moves): it’s not just for gym buffs—it’s essential medicine for our bones and beyond. During perimenopause, it counters early muscle loss (sarcopenia); in menopause, it halts the 1–2% annual decline; and post-menopause, it rebuilds what time (and hormones) have taken.
Key Effects and Benefits:
- Bone Boost: Loading bones stimulates density gains—studies show postmenopausal women can increase hip and spine strength by 1–3% yearly, directly fighting osteoporosis.
- Muscle Maintenance: Oestrogen dips erode lean mass (up to 3–5% per decade post-40), slowing metabolism and raising fall risk. Weight training preserves or builds it, enhancing balance and daily ease.
- Metabolic Magic: It regulates blood sugar, curbs midlife weight gain, and eases insulin resistance—vital as visceral fat rises.
- Whole-Body Wins: Better sleep, mood lifts (via endorphins), reduced hot flush severity, and heart health perks. Aussie experts from the Australasian Menopause Society highlight it as a top non-drug therapy for symptom relief.
Start light:
2–3 sessions weekly, 8–12 reps of compound moves like squats or rows. No gym? Home dumbbells or resistance bands work wonders.
Your 3-Move “Strong in 10 Minutes” Home Routine (2–3× per week)
- Goblet Squat (hold a heavy bag of groceries or a dumbbell) – 10–12 reps
- Push-ups on knees or against a wall – 8–12 reps
- Single-arm row (use a tin of beans or dumbbell) – 10–12 reps each side
Rest 60–90 sec between moves. Progress by adding a rep or two each week.
Fueling the Fire: The Role of Protein Intake – Protein isn’t optional—it’s the building block for muscles and bones, and menopause amps up our needs as absorption dips and repair slows.
In perimenopause, it helps stabilise weight amid hormonal chaos; during menopause, it supports training gains; post-menopause, it prevents frailty.
While collagen peptides are popular, current evidence shows they are not superior to regular dietary protein (chicken, eggs, lentils, etc.) for bone density. Save your money unless you love the taste!
Australian guidelines set the base RDI at 0.75–0.84g/kg body weight/day for women, but for midlife maintenance and activity, experts recommend 1.0–1.2g/kg—that’s about 70–84g daily for a 70kg woman. Active? Aim 1.4–1.6g/kg to maximise muscle synthesis. Prioritising protein (e.g., 25–30g per meal) can even ward off perimenopausal weight creep by curbing hunger and boosting satiety.
Easy Sources:
- Lean meats, fish, eggs (20–30g per serve).
- Plant power: Lentils, chickpeas, tofu (15–25g).
- Dairy: Greek yoghurt, cheese (10–20g).
- Snacks: Nuts, seeds, or protein shakes for quick hits.
Spread it out—post-workout is prime for recovery.
Essential Nutrients: Vitamins, Minerals, and Where to Source Them: Weight training and protein shine brighter with the right cofactors. Focus on these bone heroes, per Jean Hailes and Healthy Bones Australia—test levels with your health practitioner first, as over-supplementing isn’t wise.
- Calcium (1000–1300mg/day): The bone scaffold. Post-menopausal women need the higher end to offset loss. Sources: Whole foods like dairy (milk, yoghurt: 300mg/glass), leafy greens (kale, broccoli: 100–200mg/serve), fortified plant milks, or almonds.
- Vitamin D (600–2000 IU/day): Unlocks calcium absorption and aids muscle function. Deficiency hits up to 36% of Aussie women in winter. Sources: Sunlight (10–15 mins midday, arms/legs exposed, sans sunscreen—safely, per Cancer Council). Foods: Fatty fish (salmon: 400 IU/serve), eggs, fortified cereals.
- Magnesium (310–320mg/day): Partners with calcium for bone matrix and eases cramps/mood swings. Sources: Whole foods like spinach, nuts/seeds (pumpkin: 150mg/handful), wholegrains, dark chocolate.
More than 4 coffees or 2 standard drinks daily can increase calcium loss – easy swap: try decaf or sparkling water with lemon. Pair with Vitamin K2 (from fermented foods like natto) for directing calcium to bones, not arteries. Hydrate and limit salt to retain minerals.
Your Strong Start: Tips and Aussie Resources – Ready to lift? Begin with a check-in with your health practitioner for bone density guidance and tailor to your stage. Join free programs via Osteoporosis Australia or Jean Hailes webinars. Track progress in our community—small wins build big strength.
Menopause isn’t a slowdown—it’s your cue to get fierce.
With weight training, protein smarts, and nutrient savvy, you’re fortifying not just bones, but a vibrant life ahead.
Cheers to your power,
The Menopause & Me Team
menopauseandme.com.au
P.S. Missed our recent editions? → Embrace the Change (perimenopause, menopause & post-menopause)??
They’re all saved on the website for you anytime in the blog section
Important Disclaimer: The information in this blog/newsletter is general in nature and intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your Nurse Practitioner, doctor, or another qualified health practitioner with any questions you may have regarding a medical condition or before commencing any new treatment, exercise program, changing your diet, or taking supplements – particularly if you have existing health conditions, are on medication, or have had fractures or falls in the past. Individual needs and responses vary.
Embracing the Change: A Guide to Perimenopause, Menopause, and Post-Menopause
As we kick off our newsletter/blog series, we’re starting at the beginning – or should we say, the transition? Menopause is a natural milestone in every woman’s life, yet it’s often shrouded in myths and misinformation. Here in Australia, where the average age for menopause is 51, many of us are navigating these changes right now, with symptoms that can feel overwhelming. But here’s the empowering truth: understanding perimenopause, menopause, and post-menopause equips you to take control. We’ll unpack what these stages mean, why they happen, the common symptoms, their ripple effects on daily life, and—most importantly—how pharmacotherapy and non-pharmacological approaches can help you not just cope, but thrive. You’re not alone, and brighter days (and nights) are ahead. (click on the arrow to the left to open the full article)
The Stages: Mapping Your Menopausal Journey
Menopause isn’t a sudden switch—it’s a gradual shift across three key phases, each influenced by your body’s reproductive winding down.
- Perimenopause (The Lead-Up): This transitional phase typically starts in your 40s (sometimes earlier) and lasts 4–6 years on average, though it can stretch to 10. It’s defined by the first signs of irregular cycles—periods might be shorter, longer, heavier, or skipped altogether—as your ovaries begin to produce fewer eggs. In Australia, this stage often brings the first waves of symptoms, signaling the end of your fertile years.
- Menopause (The Turning Point): Officially, this is 12 consecutive months without a period, marking the end of ovulation and menstrual cycles. At around 51 years old for most Aussie women (ranging from 45–55), it’s a normal part of ageing, not a disease.
- Post-Menopause (The Long Haul): Everything after that final period, which could span a third of your life—up to age 80 or beyond. Hormone levels stabilise at a low baseline, and while some symptoms fade, others may linger, alongside increased health risks like osteoporosis or heart disease.
These stages vary by genetics, lifestyle, and health history. If you’ve had surgeries like a hysterectomy or treatments like chemotherapy, menopause can arrive earlier (induced menopause). (click on the arrow to the left to open the full article)
Why It Happens: The Hormone Story
At its core, this is about hormones doing their job—then slowing down. From your mid-30s, your ovaries house fewer eggs, leading to less frequent ovulation. Oestrogen, the star player for reproductive health, fluctuates wildly in perimenopause (sometimes spiking before plummeting), then drops by up to 90% by menopause. Progesterone dips too, as egg release becomes erratic, and testosterone gradually halves over decades. These shifts don’t just affect periods—they influence everything from mood to bone density. It’s biology’s way of redirecting energy from reproduction to maintenance, but the transition can feel like a bumpy ride.
Common Symptoms: What to Expect
No two journeys are identical, but many Australian women share these hallmarks, starting in perimenopause and peaking around menopause.
Physical Symptoms (affecting up to 80% of us):
- Hot flushes and night sweats: Sudden heat waves, often with sweating and chills—think chest-to-face flaring that disrupts sleep.
- Irregular periods: Unpredictable flow and timing.
- Vaginal dryness and discomfort: Thinning tissues leading to itchiness, painful sex, or urinary issues like incontinence.
- Joint aches, fatigue, and sleep disturbances: Tiredness hits hard, with 25% of women over 50 reporting poor sleep.
- Weight gain, bloating, headaches, and breast tenderness.
Emotional and Cognitive Symptoms:
- Mood swings, anxiety, irritability, or low mood: Higher depression risk, especially if you’ve had PMS before.
- Brain fog, forgetfulness, and trouble concentrating: That “mental cloudiness” many describe.
In post-menopause, flushes often ease, but dryness and bladder woes may persist. About 64% of midlife Aussie women (45–64) report bothersome symptoms in the last five years.
The Real Impact: On Work, Relationships, and Wellbeing
These changes aren’t just physical—they can shake your world. A 2023 national survey found 37% of affected women struggled with daily activities, like chores or self-care, while 31% faced work or study hurdles—17% even took extended breaks. Emotionally, 55% noted hits to mental health, with 58% of midlife women feeling the strain. Relationships suffer too: 19% reported tensions with partners, and 13% with friends or family. It’s no wonder—disrupted sleep fuels fatigue, and symptoms overlap with midlife stressors like caring for kids or ageing parents. Yet, only 61% seek professional support, often due to embarrassment (8.6%) or thinking “nothing can be done” (24%). The good news? Awareness is growing, and so are solutions.
Thriving Through It: Pathways to Relief and Renewal
Here’s where hope shines: menopause is manageable, and with the right tools, you can reclaim your vitality. Australian guidelines from the Australasian Menopause Society (AMS) and Jean Hailes emphasise personalised care—starting with lifestyle tweaks and escalating as needed. Let’s break it down.
Non-Pharmacological Therapies: Empowering Everyday Wins
These evidence-based strategies build resilience without meds, often improving overall health.
- Lifestyle Foundations: Regular exercise (aim for 30 minutes daily—walking, weights for bone health) cuts hot flushes and boosts mood. A balanced diet rich in calcium (dairy, greens, tofu) and phytoestrogens (soy) supports bones and symptoms. Ditch smoking, limit alcohol/caffeine, and layer clothes for flush management. Weight loss, if relevant, can ease multiple issues.
- Mind-Body Practices: Cognitive behavioural therapy (CBT) reduces flush bother and improves sleep/mood. Hypnosis shows promise for severity reduction. Mindfulness or paced breathing helps with anxiety—try apps tailored for menopause.
- Complementary Options: Black cohosh may rival low-dose hormones for flushes (with mood perks), per some trials. Soy isoflavones offer mild relief, but evidence is mixed—discuss with me first, especially if cancer history. Acupuncture has inconsistent but positive anecdotal support.
These aren’t cures but amplifiers: many women see 50%+ symptom relief from placebo alone, so belief matters!
Pharmacotherapy: Targeted Relief When You Need It
For moderate to severe symptoms, targeted therapies can truly transform your quality of life—backed by recommendations from the Australasian Menopause Society (AMS).
- Menopausal Hormone Therapy (MHT): Often considered the most effective option for managing hot flushes, night sweats, vaginal dryness, and supporting bone health. Whether using oestrogen-only (suitable for those who’ve had a hysterectomy) or combined with progestogen, it can provide significant relief and may even help reduce the risk of heart disease when initiated within 10 years of menopause. For most women under 60, the benefits far outweigh the risks, and we’ll tailor a discussion to your unique health profile. Topical forms are available to focus relief locally while minimising broader effects.
- Non-Hormonal Alternatives: When MHT isn’t the right fit, other prescription options like certain antidepressants or nerve-modulating medications can help ease flushes, mood changes, and sleep issues effectively.
We always start with the lowest effective approach, monitor progress closely with personalised support, and adjust as needed—many women experience meaningful improvements, paving the way for a more vibrant chapter ahead.
Your Thriving Chapter Awaits
Perimenopause, menopause, and post-menopause are chapters, not the whole story—hormonal shifts that herald wisdom and freedom. Yes, symptoms can disrupt (37% of us feel it daily), but with tools like MHT or CBT, thriving is the norm. In Australia, resources like Jean Hailes and AMS are your allies—if you wish to discuss your journey, book an appointment at menopauseandme.com.au/booking.
What’s one step you’ll take? Share in the comments or reply—we’re building this community together!
Warmly,
Menopause & Me
P.S. Next up: Building Strong Foundations! Head back next week for more information.
Insights from Jean Hailes, Australasian Menopause Society, and healthdirect—evidence-based for Aussie women.
Important Disclaimer: The information in this blog/newsletter is general in nature and intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your Nurse Practitioner, doctor, or another qualified health practitioner with any questions you may have regarding a medical condition or before commencing any new treatment, exercise program, changing your diet, or taking supplements – particularly if you have existing health conditions, are on medication, or have had fractures or falls in the past. Individual needs and responses vary.
